Ketamine
Also Known As: Ketamine, Ketanest, Ketaset, Ketalar
Ketamine is a drug used in human and veterinary medicine, mainly for starting and maintaining general anesthesia. Other uses include sedation inintensive care, as a pain killer (particularly in emergency medicine and patients with potentially compromised respiration and/or allergies to opiate and barbiturate analgesics), and treatment of bronchospasm. This drug is sometimes used recreationally. Like other drugs in its class such astiletamine and phencyclidine (PCP), ketamine is classified as a dissociative agent.[2] The state it induces is defined as "a trancelike cataleptic state characterized by profound analgesia and amnesia, with retention of protective airway reflexes, spontaneous respirations, and cardiopulmonary stability."[3] Studies have shown that respiratory function is unchanged with the administration of ketamine.[4] Though its impact on respiratory function is favorable, ketamine can still cause adverse effects which will be discussed below.
Its hydrochloride salt is sold as Ketanest, Ketaset, and Ketalar.Pharmacologically, ketamine is classified as an NMDA receptor antagonistbut does have some activity at other receptors..[5] It is on the World Health Organization's List of Essential Medicines, a list of the most important medication needed in a health system.[6]
Uses as an anaesthetic:
- Anesthesia in children, as the sole anesthetic for minor procedures or as an induction agent followed by muscle relaxant and tracheal intubation;
- Asthmatics or people with chronic obstructive airway disease;
- Emergency surgery in field conditions in war zones;
- To supplement spinal or epidural anesthesia/analgesia using low doses;
In medical settings, ketamine is usually injected intravenously orintramuscularly.[7] Since it suppresses breathing much less than most other available anaesthetics,[8] ketamine is still used in human medicine as an anesthetic; however, due to the hallucinations it may cause, it is not typically used as a primary anesthetic, although it is the anaesthetic of choice when reliable ventilation equipment is not available.
Ketamine is frequently used in severely injured patients. It is the drug of choice for patients in traumatic shock who are at risk of hypotension.[9] Hypotension is extremely dangerous in patients with severe head injury[10] and ketamine is anaesthetic agent least likely to precipitate hypotension, often even able to prevent it.[11][12] For years medical myth has held that ketamine was dangerous in patients with head injury over concerns that it might transiently increase the pressure inside the skull. This small transient effect is completely outweighed by the devastation caused by hypotension in severely head injured patients. Air medical services and paramedics are using this drug with increasing frequency.[citation needed]
Ketamine tends to increase heart rate and blood pressure. Because it tends to increase or maintain cardiac output, it is sometimes used in anesthesia for emergency surgery when the patient's fluid volume status is unknown (e.g., from traffic accidents). Ketamine can be used in podiatry and other minor surgery, and occasionally for the treatment ofmigraine. Research is ongoing in France, the Netherlands, Russia, Australia and the US into the drug's usefulness in pain therapy, depression,[13] and for the treatment of alcoholism[14] and heroin addiction.[15]
Ketamine may be used in small doses as a local anesthetic, particularly for the treatment of pain associated with movement and neuropathic pain.[16] It may also be used as an intravenous coanalgesic with opiates to manage otherwise intractable pain, particularly if this pain is neuropathic (pain due to vascular insufficiency or shingles are good examples). It has the added benefit of counteracting spinal sensitization or wind-up phenomena experienced withchronic pain. At these doses, the psychotropic side effects are less apparent and well managed withbenzodiazepines.[17] Ketamine is a coanalgesic, so is most effective when used alongside a low-dose opioid; while it does have analgesic effects by itself, the higher doses required can cause disorienting side effects.[17] The combination of ketamine with an opioid may be useful for pain caused by cancer, as suggested in animal models.[18] A review article in 2013 concluded that "despite limitations in the breadth and depth of data available, there is evidence that ketamine may be a viable option for treatment-refractory cancer pain".[19]
The effect of ketamine on the respiratory and circulatory systems is different from that of other anesthetics. When used at anesthetic doses, it will usually stimulate rather than depress the circulatory system.[20] It is sometimes possible to perform ketamine anesthesia without protective measures to the airways. Ketamine is also a potent analgesic and can be used in subanesthetic doses to relieve acute pain; however, its psychotropic properties must be taken into account. Patients have reported vivid hallucinations, "going into other worlds" or "seeing God" while anesthetized, and these unwanted psychological side effects have reduced the use of ketamine in human medicine. They can, however, usually be avoided by concomitant application of a sedative such as a benzodiazepine.[17]
Low-dose ketamine is recognized for its potential effectiveness in the treatment of complex regional pain syndrome(CRPS).[21] Although low-dose ketamine therapy is established as a generally safe procedure, reported side effects in some patients have included hallucinations, dizziness, lightheadedness and nausea. Therefore, nurses administering ketamine to patients with CRPS should do so only in a setting where a trained physician is available if needed to assess potential adverse effects on patients.[22]
In some neurological intensive care units, ketamine has been used in cases of prolonged seizures. Some evidence indicates the NMDA-blocking effect of the drug protects neurons from glutamatergic damage during prolonged seizures.[23]
As part of a cream, gel, or liquid (only available from compounding pharmacies as it is not a branded product, specific formulation and ratios are specified by the prescribing physician) for topical application for nerve pain — the most common mixture is 10% ketoprofen, 5% lidocaine, and 10% ketamine.[citation needed] Other ingredients found useful by pain specialists and their patients, as well as the compounding pharmacists who make the topical mixtures, includeamitriptyline, cyclobenzaprine, clonidine, tramadol, gabapentin, baclofen, and mepivacaine and other longer-acting local anaesthetics (e.g. tetracaine, procaine).
Ketamine is a "core" medicine in the World Health Organization's "Essential Drugs List", a list of minimum medical needs for a basic healthcare system.[24]
Emergence reactions manifest as vivid dreams, hallucinations, and delirium and occur in 12% of patients. These reactions are much less common in patients < 15 years old and > 65 years old and when administered intramuscularly. Emergence reactions can occur up to 24 hours postoperatively. The chance of this occuring can be reduced by minimizing stimulation to the patient during recovery and pretreating with a benzodiazepine. If given a benzodiazepine, a lower dose of ketamine than normal should be given. Patients who experience severe reactions may require treatment with a small dose of a short or ultra-short acting barbiturate.[36] Tonic-clonic movements are reported at higher anesthetic doses in greater than 10% of patients.[37] As discussed below, current research suggests that acute ketamine exposure does not cause significant neurotoxicity. Long term[edit]Because ketamine is not administered chronically in a typical clinical setting, long-term effects are primarily reported and investigated in recreational ketamine users and in animal models.[38] Neurological effects[edit]In 1989, psychiatry professor John Olney reported ketamine caused irreversible changes in two small areas of the rat brain, which, however, has significant differences in metabolism from the human brain, so may not occur in humans.[39][40][41][42] Indeed, a review published in 2009 found no evidence of ketamine-induced neuron death in humans.[43] The first large-scale, longitudinal study of ketamine users found that current frequent ketamine users (at least 4 days/week, averaging 20 days/month) had increased depression and impaired memory by several measures, including verbal, short-term memory and visual memory. However, current infrequent (1–4 days/month, averaging 3.25 days/month) ketamine users and former ketamine users were not found to differ from controls in memory, attention and psychological well-being tests. This suggests the infrequent use of ketamine does not cause cognitive deficits, and that any deficits that might occur may be reversible when ketamine use is discontinued. However, abstinent, frequent, and infrequent users all scored higher than controls on a test of delusional symptoms.[44] Short-term exposure of cultures of GABAergic neurons to ketamine at high concentrations led to a significant loss of differentiated cells in one study, and non-cell-death-inducing concentrations of ketamine (10 μg/ml) may still initiate long-term alterations of dendritic arbor in differentiated neurons. The same study also demonstrated chronic (>24 h) administration of ketamine at concentrations as low as 0.01 μg/ml can interfere with the maintenance of dendritic arbor architecture. These results raise the possibility that chronic exposure to low, subanesthetic concentrations of ketamine, while not affecting cell survival, could still impair neuronal maintenance and development.[45][46] More recent studies of ketamine-induced neurotoxicity have focused on primates in an attempt to use a more accurate model than rodents. One such study administered daily ketamine doses consistent with typical recreational doses (1 mg/kg IV) to adolescent cynomolgus monkeys for varying periods of time.[47] Decreased locomotor activity and indicators of increased cell death in the prefrontal cortex were detected in monkeys given daily injections for six months, but not those given daily injections for one month.[47] A study conducted on rhesus monkeys found that a 24-hourintravenous infusion of ketamine caused signs of brain damage in 5-day-old but not 35-day-old animals.[48] Some neonatal experts do not recommend the use of ketamine as an anesthetic agent in human neonates because of the potential adverse effects that it may have on the developing brain. These neurodegenerative changes in early development have been seen with other drugs that share the same mechanism of action of NMDA receptor antagonism as ketamine.[49] The acute effects of ketamine cause cognitive impairment including reduced vigilance, verbal fluency, short-term memory, and executive function, as well as schizophrenia-like perceptual changes.[50] Urinary tract effects[edit]According to a recent systematic review, 110 documented reports of irritative urinary tract symptoms from ketamine dependence exist.[51] Urinary tract symptoms have been collectively referred as "ketamine-induced ulcerative cystitis" or "ketamine-induced vesicopathy", and they include urge incontinence, decreased bladder compliance, decreased bladder volume, detrusor overactivity, and painful haematuria (blood in urine). Bilateral hydronephrosis and renal papillary necrosis have also been reported in some cases.[38][51] The pathogenesis of papillary necrosis has been investigated in mice, and mononuclear inflammatory infiltration in the renal papilla resulting from ketamine dependence has been suggested as a possible mechanism.[52] The time of onset of lower urinary tract symptoms varies depending, in part, on the severity and chronicity of ketamine use; however, it is unclear whether the severity and chronicity of ketamine use corresponds linearly to the presentation of these symptoms. All reported cases where the user consumed greater than 5 grams per day reported symptoms of the lower urinary tract.[51] Urinary tract symptoms appear to be most common in daily ketamine abusers who have abused the drug for an extended period of time.[38] These symptoms have presented in only one case of medical use of ketamine. However, following dose reduction, the symptoms remitted.[38] Management of these symptoms primarily involves ketamine cessation, for which compliance is low. Other treatments have been used, including antibiotics, NSAIDs, steroids, anticholinergics, and cystodistension.[51] Both hyaluronic acidinstillation and combined pentosan polysulfate and ketamine cessation have been shown to provide relief in some patients, but in the latter case, it is unclear whether relief resulted from ketamine cessation, administration of pentosan polysulfate, or both. Further follow-up is required to fully assess the efficacy of these treatments.[51] Case reports of hepatotoxicity in chronic pain management[edit]In case reports of three patients treated with (S)-(+)-ketamine for relief of chronic pain, liver enzyme abnormalities occurred following repeat treatment with ketamine infusions, with the liver enzyme values returning below the upper reference limit of normal range on cessation of the drug. The result suggests liver enzymes must be monitored during such treatment.[53] Interactions[edit]Other drugs which increase blood pressure may interact with ketamine in having an additive effect on blood pressure including: stimulants, SNRI anti-depressants, MAOIs. Increase blood pressure, increased heart rate, palpitations and arrhythmias may be potential effects. Ketamine alone additionally increases intracranial pressure (ICP) Ketamine may increase the effects of other sedatives, including but not limited to: benzodiazepines, barbiturates,opiates/opioids, anesthetics, and alcoholic beverages.[citation needed] Mechanism of action[edit]Central nervous system[edit]Ketamine is a noncompetitive NMDA receptor (NMDAR) antagonist. It appears to inhibit the receptor by binding both in the open channel and at an allosteric site.[54] The S(+) and R(-) stereoisomers bind with different affinities: Ki = 3200 and 1100 nM, respectively.[55] NMDAR antagonism results in analgesia by preventing central sensitization in dorsal horn neurons; in other words, ketamine's actions interfere with pain transmission in the spinal cord.[37] Ketamine also inhibits nitric oxide synthase, inhibiting production of nitric oxide, a neurotransmitter involved in pain perception, and hence further contributing to analgesia.[56] It also interacts with sigma and opioid receptors, but with lower affinity and without significantly contributing to analgesia.[57] Ketamine also interacts with a host of other receptors to effect analgesia. It blocks voltage-sensitive calcium channels and depresses sodium channels, attenuating hyperalgesia; it alters cholinergic neurotransmission, which is implicated in pain mechanisms; and it acts as a noradrenaline and serotonin uptake inhibitor, which are involved in descendingantinociceptive pathways.[37][58] Peripheral systems[edit]Ketamine affects catecholaminergic transmission as noted above, producing measurable changes in peripheral organ systems, including the cardiovascular, gastrointestinal, and respiratory systems:[56]
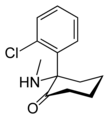
Chemical structure[edit]Ketamine is a chiral compound. Most pharmaceutical preparations of ketamine are racemic; however, some brands reportedly have (mostly undocumented) differences in their enantiomeric proportions. The more active enantiomer, (S)-ketamine, is also available for medical use under the brand name Ketanest S.[59]
Pharmacology[edit]Pharmacokinetics[edit]Ketamine is absorbable via intravenous, intramuscular, oral, and topical routes due to both its water and lipid solubilities.[60] When administered orally, it undergoes first-pass metabolism, where it is biotransformed in the liver byCYP3A4 (major), CYP2B6 (minor), and CYP2C9 (minor) isoenzymes into norketamine (through N-demethylation) and finally dehydronorketamine.[61] Intermediate in the biotransformation of norketamine into dehydronorketamine is thehydroxylation of norketamine into 5-hydroxynorketamine by CYP2B6 and CYP2A6. Dehydronorketamine, followed by norketamine, is the most prevalent metabolite detected in urine.[62] As the major metabolite of ketamine, norketamine is one-third to one-fifth as potent anesthetically, and plasma levels of this metabolite are three times higher than ketamine following oral administration.[60][63] Bioavailability through the oral route reaches 17–20%; bioavailability through other routes are as follows: 93% intramuscularly, 25–50% intranasally, 30% sublingually, and 30% rectally.[37][61] Peak plasma concentrations are reached within a minute intravenously, 5–15 min intramuscularly, and 30 min orally.[63]Ketamine's duration of action in a clinical setting is 30 min to 2 h intramuscularly and 4–6 h orally.[37] Plasma concentrations of ketamine are increased by diazepam and other CYP3A4 inhibitors.[37] Pharmacodynamics[edit]Pharmacologically, ketamine is classified as an NMDA receptor antagonist.[5] At high, fully anesthetic level doses, ketamine has also been found to bind to μ-opioid receptors type 2 in cultured human neuroblastoma cells – however, without agonist activity[64] – and to sigma receptors in rats.[65] Ketamine also interacts with muscarinic receptors, descending monoaminergic pain pathways and voltage-gated calcium channels,[66] and it inhibits hyperpolarization-activated cyclic nucleotide–modulated (HCN1) cation channels.[67]
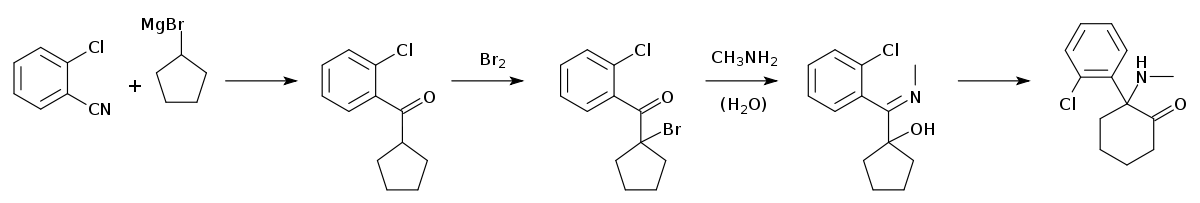
Synthesis[edit]Ketamine is synthesized from 2-chlorobenzonitrile, which reacts with the Grignard reagent cyclopentylmagnesium bromide to give 1-(2-chlorobenzoyl)cyclopentane.[68][69] The next step is bromination using bromine to the corresponding bromoketone, which upon reaction with an aqueous solution of methylamine forms the methylimino derivative. During this reaction, a simultaneous hydrolysis of the tertiary bromine atom occurs. On heating the reaction product in decalin, a ring-expansion rearrangement occurs, forming ketamine. History[edit]Medical use[edit]Ketamine was originally developed in 1962 as a derivative of phencyclidine(PCP), which was synthesized in 1926, a feat made possible by the discovery of a new organic Grignard reaction by Parke-Davis scientist Harold Maddox.[70]Initially known as CI-581, ketamine was first synthesized by Parke-Davis scientist Calvin Stevens. Pharmacological investigations in human subjects began in 1964.[70] These investigations demonstrated that ketamine's shorter duration of action and lesser psychotomimetic profile made it favorable over PCP as a "dissociative" anesthetic.[71] Following FDA approval in 1970, ketamine anesthesia was first given to American soldiers during the Vietnam War.[72] Nonmedical use[edit]Main article: Recreational use of ketamine
Nonmedical use of ketamine began on the West Coast of the United States in the early 1970s.[72] Early use was documented in underground literature such as The Fabulous Furry Freak Brothers. It was used in psychiatric and other academic research through the 1970s, culminating in 1978 with the publishing of psychonaut John Lilly's The Scientistand Marcia Moore and Howard Alltounian's Journeys into the Bright World, which documented the unusual phenomenology of ketamine intoxication.[73] The incidence of nonmedical ketamine use increased through the end of the century, especially in the context of raves and other parties.[74][75][76][77][78] However, its emergence as a club drugdiffers from other club drugs (e.g. MDMA) due to its anesthetic properties (e.g., slurred speech, immobilization) at higher doses;[78] in addition, reports of ketamine being sold as "ecstasy" are common.[79] The use of ketamine as part of a "post-clubbing experience" has also been documented.[80] Ketamine's rise in the dance culture was most rapid inHong Kong by the end of the 1990s.[78] Related to its purported ability to cause confusion and amnesiac effects, ketamine can leave users vulnerable to drug-facilitated sexual assault.[81] Society and culture[edit]Legal status[edit]The increase in illicit use prompted ketamine's placement in Schedule III of the United States Controlled Substance Actin August 1999.[82] In the United Kingdom, it became labeled a Class C drug on 1 January 2006.[62][83] On 10 December 2013 the UKACMD recommended that the government reclassify ketamine to become a Class B drug,[84] and on 12 February 2014 the Home Office announced they would follow this advice "in light of the evidence of chronic harms associated with ketamine use, including chronic bladder and other urinary tract damage".[85][86] The UK Minister of State for Crime Prevention, Norman Baker, responding to the ACMD's advice said that the issue of its recheduling for medical and veterinary would be addressed "separately to allow for a period of consultation."[85] In Canada, ketamine is classified as a Schedule I narcotic, as of August 2005.[87] In Hong Kong, as of 2000, ketamine is regulated under Schedule 1 of Hong Kong Chapter 134 Dangerous Drugs Ordinance. It can only be used legally by health professionals, for university research purposes, or with a physician's prescription.[88] By 2002, ketamine was classified as schedule III in Taiwan; given the recent rise in prevalence in East Asia, however, rescheduling into schedule I or II is being considered.[62] In December 2013 the government of India added ketamine to Schedule X of the Drug and Cosmetics Act, adding restrictions on who can buy or sell it.[89] International brand names[edit]Brand names for ketamine vary internationally:[90]
Research[edit]Antidepressant use[edit]Animal studies[edit]Some research in rodents has attributed the effects of ketamine to being an NMDA receptor antagonist,[54] which increases the activity of the AMPA receptor, and this boost in AMPA activity may be crucial for ketamine’s rapid antidepressant actions.[91] NMDA and AMPA are receptors for the neurotransmitter glutamate. The glutamate system is an emerging target for antidepressant drug discovery and development.[92][93][94] Acute administration of ketamine at the higher dose, but not imipramine, increased BDNF protein levels in the rathippocampus. The increase of hippocampal BDNF protein levels induced by ketamine might also be necessary to produce a rapid onset of antidepressant action in rats.[95] Human studies[edit]Research on the antidepressant effects of ketamine infusions at subanaesthetic doses has consistently shown rapid (4 to 72 hours) responses from single doses, with substantial improvement in mood in the majority of patients andremission in some. However, these effects are often short-lived, and attempts to prolong the antidepressant effect with repeated doses and extended ("maintenance") treatment have resulted in only modest success.[96] When treating patients suffering from complex regional pain syndrome (CRPS) with a low-dose (subanesthetic) ketamine infusion, some patients were observed in the early 2000s to make a significant recovery from depression. This recovery was not formally documented, as the primary concern was pain management and it was not possible to quantify to what degree depression recovery was secondary to the patient's recovery from CRPS.[97] This led the investigators to conduct a study in two patients with severe depression, with the dose carefully monitored to prevent hallucinogenic side effects. The patients demonstrated significant, long-term improvement.[97] A randomized placebo-controlled study in 18 patients conducted at the US NIH and published in 2006, found ketamine significantly improved treatment-resistant major depression within hours of injection that lasted up to one week after the single dose.[98] NIMH director Dr. Thomas Insel remarked:"To my knowledge, this is the first report of any medication or other treatment that results in such a pronounced, rapid, prolonged response with a single dose. These were very treatment-resistant patients."[99] A 2013 two-site randomized controlled clinical trial of ketamine in patients with treatment-resistant depression found that 64% of the patients responded after 24 hours according to the Montgomery–Åsberg Depression Rating Scale compared to 28% responding to midazolam.[100] A 2014 study found that a series of three or six ketamine infusions had a rapid antidepressant effect in treatment-resistant depression (TRD). 29% of a small sample responded, in a period ranging from six hours to the third infusion; beneficial effects lasted from 25 to 168 days. Some test subjects suffered acute adverse reactions during the infusion (7%) or failure to benefit and increasing anxiety (18%). Ketamine was not associated with memory impairment.[101] Kudoh et al. investigated whether ketamine is suitable for depressed patients who had undergone orthopedic surgery.[102] Depressed mood, suicidal tendencies, somatic anxiety, and hypochondriasis significantly decreased in the active group as compared with the control. The group receiving ketamine also had significantly lower postoperative pain. |